Get Expert Advice from Top Surgeons! Schedule Your Consultation.
Get The Best Endometriosis Treatment At GEM Hospital

GEM Hospital offers specialized endometriosis treatment services to help patients manage their symptoms and improve their quality of life. Trust our expert medical team for comprehensive care and effective treatment options.
-
Trusted Expertise
-
Precise Diagnostics
-
Advanced Treatments
-
Quality Care
-
24/7 Assistance
Endometriosis: Redefining Pain, Reclaiming Life
Preface
In a world where health issues are often discussed openly, endometriosis remains shrouded in silence and misunderstanding. For millions of people, this condition is not just a medical diagnosis but a daily battle marked by pain, uncertainty, and isolation. It is our hope that this book will shed light on the realities of living with endometriosis, fostering understanding and connection among those affected.
Endometriosis can affect any woman, yet many endure the symptoms without a proper diagnosis or support. Through personal stories, expert insights, and practical advice, we aim to empower readers to advocate for themselves and seek the care they deserve.
In these pages, you will find a comprehensive exploration of endometriosis—from the intricacies of its biology to the emotional impact it has on mental health. We will delve into the latest research, treatment options, and coping strategies, all while emphasising the importance of community and solidarity.
As you read, we encourage you to embrace your journey, however complex it may be. You are not alone in this fight. Together, we can raise awareness, break the stigma, and foster a more informed and compassionate care about endometriosis. Here, we present to you the testimonials of patients with endometriosis who have connected with us and gained successful treatment, support, lifestyle adjustments and living a fulfilling life despite the condition.
Our team of gynecologists specializes in the laparoscopic treatment of endometriosis. Recognizing the need for dedicated care, we are launching a clinic focused exclusively on endometriosis. This clinic aims to provide comprehensive and holistic treatment options for patients.
The purpose of this publication is to raise public awareness about the condition. The book will cover various aspects of endometriosis, including its diagnosis, treatment options, and the benefits of a holistic approach to care.
This book remarks the start of the individualised care for patient with endometriosis by initiating the endometriosis clinic in GEM hospital, Coimbatore. Thank you for joining us on this important journey. Let’s embark on this path of understanding, healing, and hope together.
ENDOMETRIOSIS
Endometriosis is a medical condition in which tissue similar to the lining of the uterus, called endometrium, grows outside the uterus. This can occur on the ovaries, fallopian tubes, the outer surface of the uterus, and other organs within the pelvis or outside of pelvis as well.
Pathophysiology:
The endometrial-like tissue outside the uterus behaves similarly to the tissue inside the uterus. It thickens, breaks down, and bleeds with each menstrual cycle. However, unlike the endometrial tissue that exits the body during menstruation, this displaced tissue has no way to leave the body. This leads to inflammation, pain, and the formation of scar tissue (adhesions).
Symptoms:
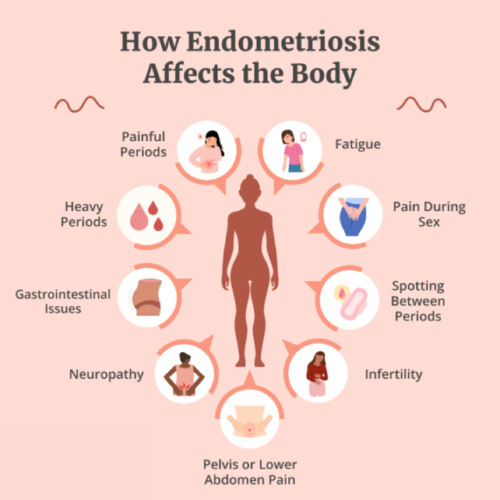
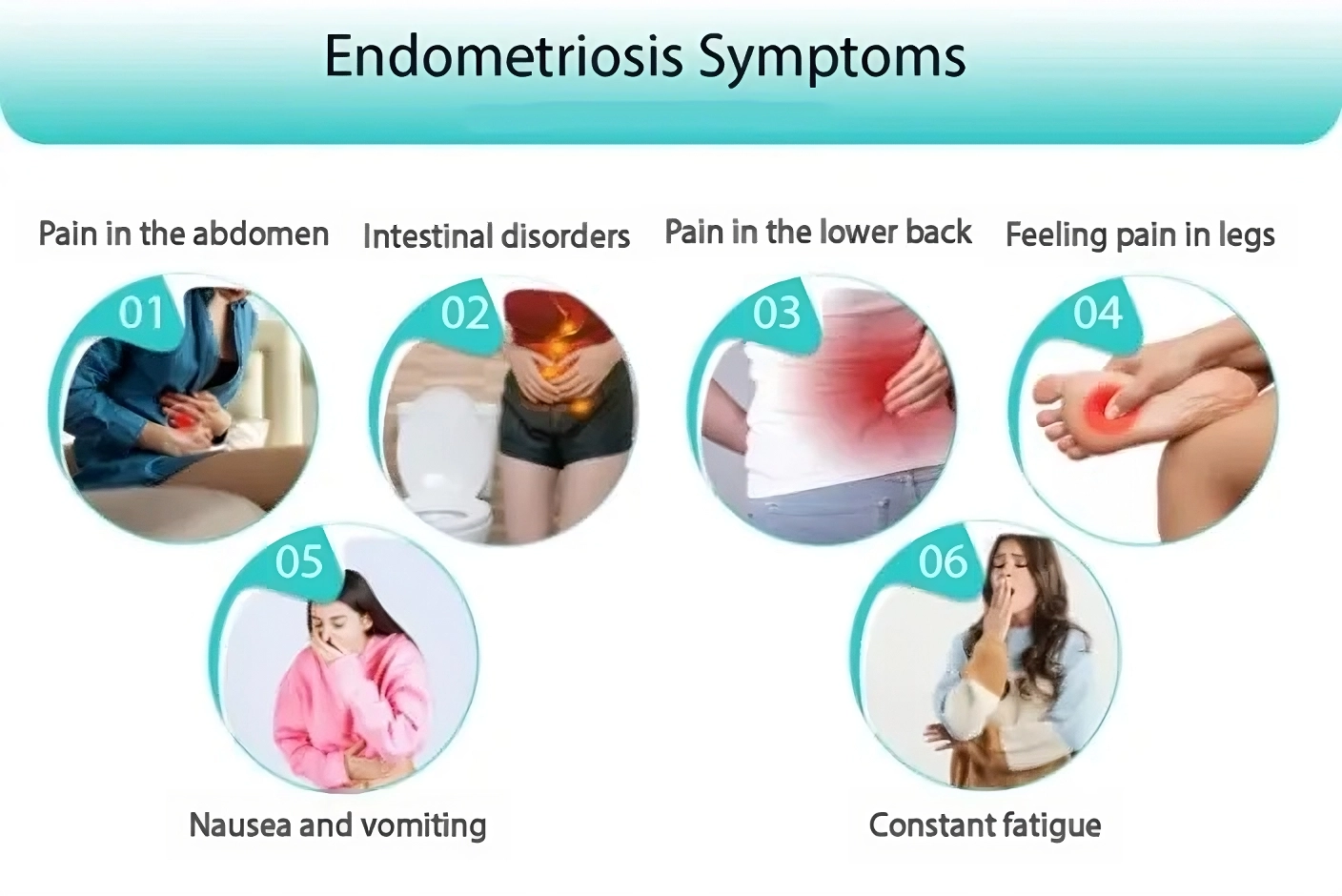
The symptoms of endometriosis can vary but often include:
-
Pelvic pain: Often associated with menstrual periods, but it can also occur at other times.
-
Dysmenorrhea: Painful periods that are more severe than usual.
-
Dyspareunia: Pain during or after sex.
-
Dyschezia: Pain with bowel movements or urination, especially during menstrual periods.
-
Menorrhagia: Heavy menstrual bleeding or bleeding between periods.
-
Infertility: Endometriosis is sometimes first diagnosed in those seeking treatment for infertility.
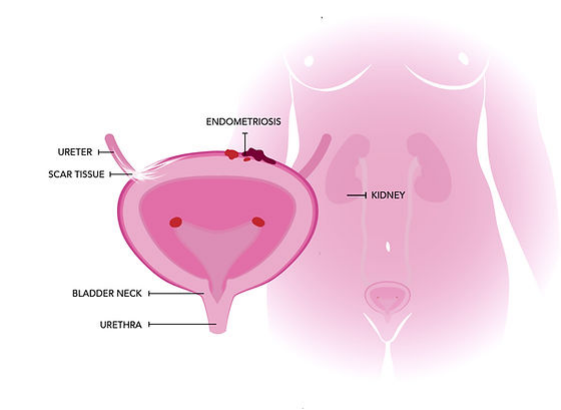
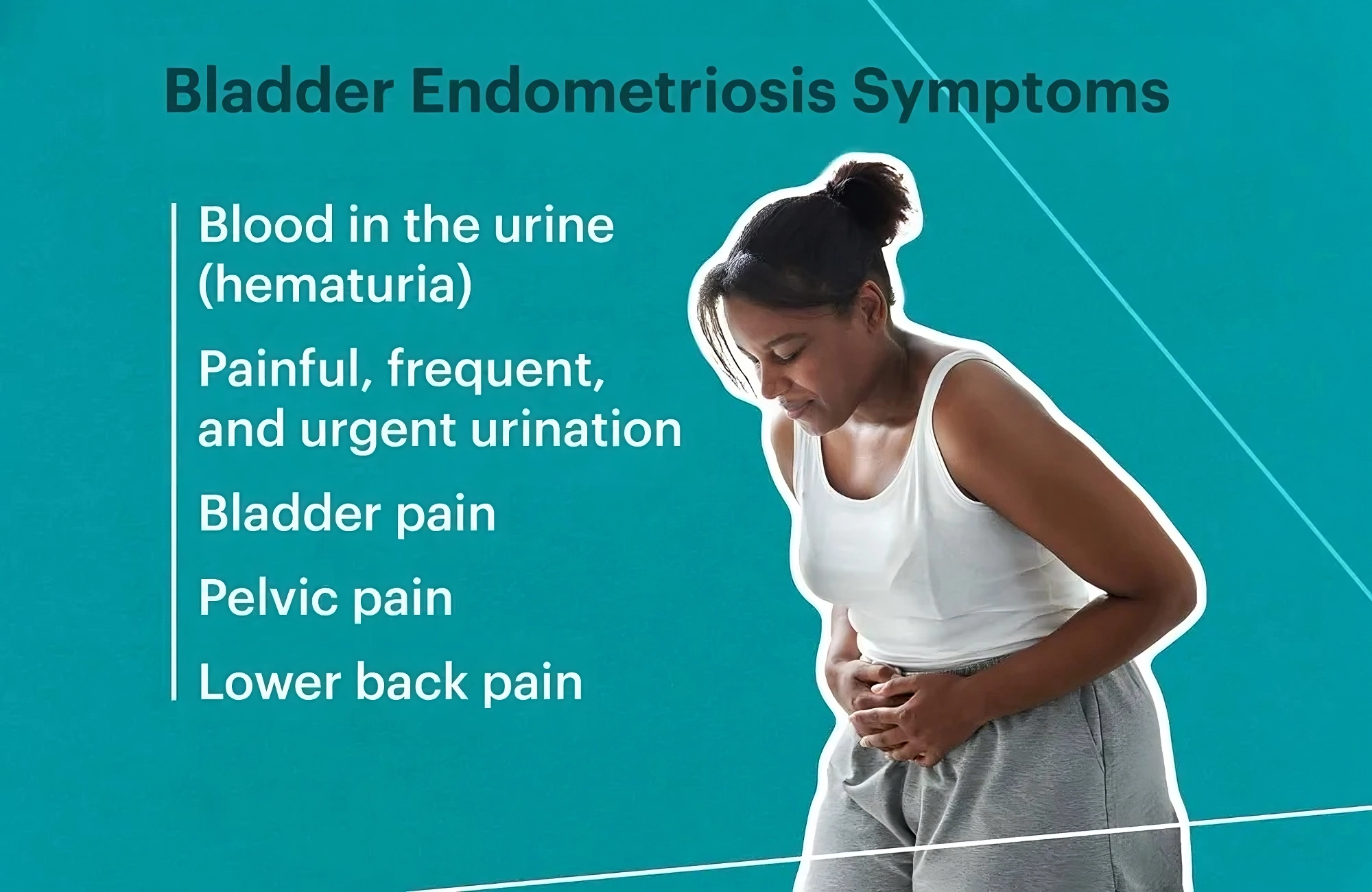
Bladder endometriosis
Bladder endometriosis occurs when endometrial-like tissue (similar to the lining of the uterus) grows on or around the bladder. This is a form of pelvic endometriosis and can cause a variety of urinary symptoms. It is less common than other forms of endometriosis but can still significantly affect a woman's quality of life
Symptoms of bowel endometriosis:
Symptoms of bladder endometriosis:
-
Painful Urination (Dysuria):
-
Increased Urinary Frequency
-
Urgency to Urinate
-
Blood in Urine (Hematuria)
-
Pelvic Pain or Lower Abdominal Pain
-
Painful Intercourse (Dyspareunia):
-
Bloating and Gastrointestinal Discomfort
Bowel Endometriosis
Bowel Endometriosis is a form of endometriosis where tissue similar to the lining of the uterus (endometrium) grows on or around the bowel (intestines). This condition is part of pelvic endometriosis, and it can cause a range of gastrointestinal and pelvic symptoms, sometimes mimicking other digestive disorders. It can be more difficult to diagnose due to its overlap with other conditions like irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD).
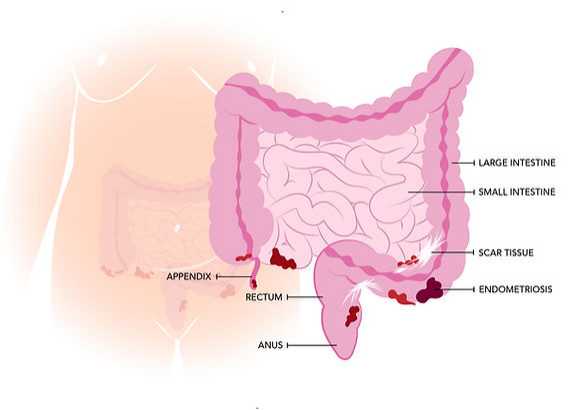
Common Symptoms of Bowel Endometriosis
-
Painful Bowel Movements
-
Diarrhoea or Constipation
-
Bloating and Abdominal Distension
-
Nausea
-
Painful Intercourse (Dyspareunia)
-
Lower Abdominal and Pelvic Pain
-
Blood in Stool
-
Fatigue
Causes and Risk Factors:
The exact cause of endometriosis is not well understood, but several theories exist:
-
Retrograde menstruation: Menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body.
-
Embryonic cell transformation: Hormones such as estrogen may transform embryonic cells into endometrial-like cell implants during puberty.
-
Surgical scars: After surgeries such as a hysterectomy or C-section, endometrial cells may attach to the surgical incision.
-
Immune system disorders: Problems with the immune system may make the body unable to recognize and destroy endometrial-like tissue growing outside the uterus.
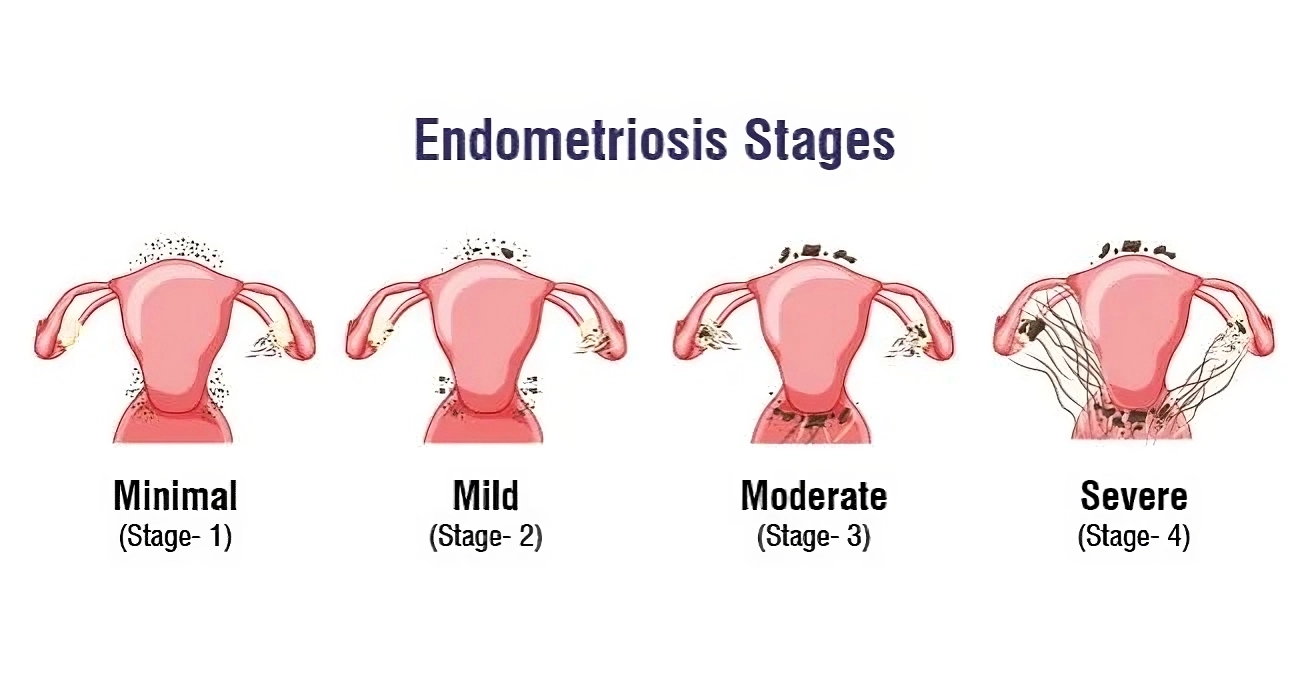
Stages of endometriosis:
APPROACH TO PATIENT WITH ENDOMETRIOSIS
The approach to managing a patient with endometriosis is indeed unique and multifaceted, as it involves not just the physical symptoms but also emotional and psychological well-being. Here are key aspects of this individualized approach:
-
Comprehensive Assessment
-
Multidisciplinary Team
-
Symptom Management
-
Fertility Considerations
-
Surgical Options
-
Education and Support
-
Regular Follow-up
-
Psychosocial Support
This comprehensive and patient-centered approach helps ensure that the management of endometriosis is tailored to each individual's unique circumstances, enhancing their quality of life and overall well-being.
DIAGNOSIS:
-
The diagnostic delay of endometriosis is a hallmark of a disease.
-
Laparoscopic identification of endometriotic lesions with histological verification has been described as the diagnostic gold standard.
-
Other factors may contribute to the delay includes lack of awareness.
CAN CLINICAL SYMPTOMS PREDICT THE PRESENCE OF ENDOMETRIOSIS?
-
Women with subsequent diagnosis of endometriosis had higher proportion of abdomino pelvic pain or heavy menstrual bleeding.
-
cyclical and non-cyclical signs and symptoms: dysmenorrhea, heavy menstrual bleeding, deep dyspareunia/postcoital bleeding, dysuria, dyschezia, painful rectal bleeding or haematuria, shoulder tip pain, catamenial pneumothorax, cyclical cough/ haemoptysis/chest pain, cyclical scar swelling and pain, fatigue, and infertility.
-
In addition, history of being diagnosed with an ovarian cyst with irritable bowel syndrome, with pelvic inflammatory disease or with fibrocystic breast disease were risk factors for subsequent diagnosis of endometriosis.
-
Increasing the number of symptoms increased the chance of having endometriosis.
Endometriosis can be challenging to diagnose due to its varied symptoms and similarities to other conditions. Here are the primary techniques used for diagnosis:
1. Medical History and Symptoms Review: A thorough discussion of symptoms, menstrual history, and family history helps identify potential endometriosis.
2. Pelvic Examination: A healthcare provider may perform a pelvic exam to feel for abnormalities, such as cysts or scar tissue. Clinical examination, including vaginal examination where appropriate, should be considered to identify deep nodules or endometriomas in patients with suspected endometriosis, although the diagnostic accuracy is low.
3. Imaging Tests:
-
Ultrasound: Transvaginal ultrasound can help identify endometriomas (cysts formed from endometriosis) and assess pelvic anatomy.
-
MRI: Magnetic resonance imaging provides detailed images of the pelvic organs and can help identify the extent of endometriosis.
In patients with negative imaging results or where empirical treatment was unsuccessful or inappropriate, the GDG recommends that clinicians consider offering laparoscopy for the diagnosis and treatment of suspected endometriosis.
4. Laparoscopy: This is a surgical procedure considered the gold standard for diagnosing endometriosis. A laparoscope is inserted through small incisions in the abdomen, allowing direct visualization of endometrial tissue outside the uterus. Biopsies can also be taken during this procedure.
5. Histopathological Examination: Tissue samples obtained during laparoscopy can be examined under a microscope to confirm the presence of endometrial-like tissue.
6. Blood Tests: While not definitive for diagnosis, certain blood tests, like CA-125, may be used to assess for endometriosis. Elevated levels can suggest endometriosis, but they can also indicate other conditions.
7. Symptom Scoring Systems: Some clinicians use validated questionnaires and scoring systems to assess symptom severity and impact on quality of life, aiding in diagnosis and treatment planning.
A combination of these methods is often used to achieve an accurate diagnosis. If you suspect endometriosis, consulting a healthcare provider is crucial for proper evaluation and management.
TREATMENT:
-
Endometriosis cannot be cured, only managed through a number of treatments
-
Medications can only provide a short time relief of pain, which means that most endo sufferers will have to undergo multiple surgeries in their lifetime
-
Endometriosis, if found at an early stage, can be more easily treated and prevented from progressing
MANAGEMENT
Short term goals
-
Relief of pain
-
Improvement of fertility
Long term goals
-
Prevention of disease progression and
-
Prevention of recurrence after therapy
SURGICAL TREATMENT:
Indications: Individualised, based on the symptoms and signs in each patient and it is tailor made.
-
Pain not relieved with medical management
-
Improvement of fertility, ovarian endometrioma
-
Significant symptoms affecting quality of life
Goal:
-
Remove all visible disease
-
Release all adhesions
-
To restore normal anatomy
SURGICAL MANAGEMENT OF ENDOMETRIOSIS:
The primary surgical options:
1. Laparoscopy: This minimally invasive surgery is the most common approach for diagnosing and treating endometriosis. It allows surgeons to remove endometrial implants, cysts, and adhesions can be excised or vaporized. Lysis of Adhesions, scar tissue that binds organs together can be cut to restore normal anatomy.
2. Hysterectomy: For women with severe endometriosis who have not responded to other treatments and do not wish to preserve fertility, a hysterectomy (removal of the uterus) may be considered. This can be accompanied by:
3. Oophorectomy: Removal of one or both ovaries, which can reduce estrogen levels and may alleviate symptoms.
4. Presacral Neurectomy: This procedure involves cutting the nerves that transmit pain signals from the uterus and can be considered for patients with chronic pelvic pain.
5. Fertility Surgery: For those trying to conceive, surgical treatment can improve fertility by removing endometrial tissue and restoring normal anatomy.
6. Nerve Block Procedures: In some cases, addressing nerve pain through specific surgical interventions may be beneficial.
Considerations and complications:
-
Recurrence: Even after surgical treatment, endometriosis can recur, so ongoing management and monitoring may be necessary.
-
Pain Relief vs. Fertility: The choice of procedure often depends on whether the primary goal is pain relief or preserving fertility.
-
Multidisciplinary Approach: Collaboration with specialists, such as gynecologists and pain management experts, can enhance treatment outcomes.
It is essential that patient gets to discuss all options with her doctor, potential risks and benefits with their healthcare provider to determine the most appropriate surgical management for their specific situation.
Factors determining type of surgery
-
Age
-
Stage of disease
-
Severity of pain
-
Associated infertility
-
Prior medical treatment
Postoperative Hormonal therapy in endometriosis
It is important for patients to schedule follow-up appointments after surgery to monitor their recovery and address any concerns. To reduce the risk of endometriosis recurrence, we recommend hormonal therapy options such as Oral progesterones, GnRH agonists/ antagonists and the levonorgestrel intrauterine system (LNG-IUS). These treatments can help manage symptoms, supporting long-term health. Please ensure you adhere to the follow-up schedule and discuss any questions you may have about your treatment plan.
PSYCHOLOGICAL IMPLICATIONS
-
Fear of never being free from pain, never getting pregnant, or having a normal life
-
Depression
-
Decreased sex drive because mere anticipation of pain during intercourse can made sex even more painful by increasing anxiety
-
Doubts about sexuality
-
Poor self image
-
Knowledge will give hope and control
-
Education is an empowering tool by which women are enabled to cope with the disease
-
Suffering in silence, need support networks
Endometriosis can significantly impact mental health. The chronic pain and challenges associated with the condition often lead to feelings of anxiety, depression, and frustration. Here are some key points to consider:
Fueling a Healthy Start: The Power of Lifestyle Choices
1. Pain and Symptoms: Chronic pain from endometriosis can be debilitating, affecting daily life and leading to emotional distress.
2. Diagnosis Journey: The often lengthy and challenging process of getting a diagnosis can contribute to feelings of isolation and hopelessness.
3. Social Impact: Endometriosis can affect relationships, work, and social activities, leading to further emotional strain.
4. Coping Strategies: Mental health support, such as therapy, support groups, and stress management techniques, can be beneficial. Mindfulness, exercise, and hobbies may also help alleviate symptoms.
5. Medical Support: It's important for individuals with endometriosis to communicate openly with healthcare providers about both physical and mental health needs.
Seeking support and addressing both the physical and emotional aspects of endometriosis is crucial for overall well-being.
MYTHS ABOUT ENDOMETRIOSIS:
Endometriosis is the Career Woman’s disease
-
Financial resources of middle class women gave them the opportunity to be diagnosed more often than women of lower class standings
-
Endometriosis does not discriminate, it is found in every socio-economic class and in every ethnic group
Endometriosis only affects women in their reproductive years
-
While it initially strikes in reproductive years, it can progress into menopause
Pregnancy cures Endometriosis
-
may trigger a remission of the disease for a time, but it does not get rid of it completely
-
researchers found that there was a recurrence of endometriosis symptoms about 10 months after pregnancy
-
endometriosis is one of the leading causes of female infertility, so a woman may not be able to get pregnant at all
Menstrual pain is mostly psychogenic (in your head)
-
endometriosis is a complicated, excruciatingly painful disease
-
it involves a high amount of physical and emotional torment
Hysterectomy cures Endometriosis
-
women are misled to believe that after a hysterectomy their pain will go away
-
the disease could already have spread to the non reproductive organs as well
This Endometriosis Clinic is among the few centres in India providing top-notch laparoscopic surgery for gynaecological disorders, allowing patients to avoid traditional laparotomy that typically require extended hospital stays and longer recovery periods.
Our skilled multi-disciplinary team is led by Dr. Kavitha Yogini , HOD, Department of Endogynecology, GEM hospital, laparoscopic surgeon with extensive experience. Her expertise guarantees that patients receive exceptional care in a compassionate setting.
The Endometriosis Clinic features one of the India’s premier multi-disciplinary teams, composed of experts in gynaecology, general and colorectal surgery, urology and hepatobiliary surgery, and pain management, alongside a fully qualified registered nurse.
The endometriosis clinic was founded by Dr. C Palanivelu.
We offer a comprehensive approach to endometriosis treatment through a multi-disciplinary team of highly skilled specialists.
Our process includes confirming your diagnosis and discussing various therapeutic options, including the severity staging of your condition. We primarily use laparoscopic techniques, which are effective in 99-100 % of cases, to provide long-term symptom relief.
Our team is equipped to handle even the most complex surgeries, often collaborating with gynaecological, urological, and colorectal surgeons. Additionally, we have a Consultant Anaesthetist with a specialized focus on Pain Management.
Meet our team of skilled doctors